Eating for your health and your budget
Eating to control your blood glucose can seem difficult when you are on a tight budget. The good news is that there are many affordable nutritious choices. Taking time to plan and shop wisely allows you to make the most of your food dollar.
Plan ahead
Meal planning can save money and help you buy healthy foods for yourself and your family. Before you go shopping, plan your meals and snacks for the next week.
- Check the flyer each week, for sale items to help you build your meal plan.
- Plan for three meals at regular times each day to help control your blood glucose. Balance your meals by following the healthy plate from Canada’s Food Guide https://food-guide.canada.ca/en/.
- Plan to have healthy snacks on hand for when you need them. Consider some portable snack options for days that you are on the go.
- Think about what you can make yourself, since ready-to-eat foods usually cost more.
- Reduce Food waste by using leftovers for another meal, you can also freeze and reheat leftovers on busy days.
Make a grocery list
Go to the grocery store armed with a list of the foods you will need for the next week. Following the list helps you avoid buying extra foods that you do not really need.
- Keep a list on your fridge. Jot down items as they run low.
- Check the fridge, freezer and cupboards to see what you have.
- Use your meal plan to make your list.
- Write your list according to the layout of the store, buy items that are not on your list, only if they are a very good deal.
Shop smart
- Remember your list – tuck it in your wallet or store it on your phone.
- Make time to grocery shop. You will do a better job of comparing prices when you are less rushed.
- Do not shop when you are hungry or tired. Items look much more appealing when you are really hungry.
- Spend less on highly processed foods like pop, chips, cookies and candies. They add to your food bill, provide little nutritional value, and may also raise your blood glucose.
- Buy store brands. They are often less expensive than brand names.
- Use the unit price shown on the shelf tags to compare the price of different sized packages. Larger packages may be a better deal, although you will only save money if you use, freeze or preserve the food before it spoils.
- Check best before dates and plan to use products before they expire.
Try different protein sources
- Choose more affordable options such as eggs, peanut butter, beans, lentils and other legumes are inexpensive protein foods. Use them in your meals several times a week.
- Find recipes that use less expensive cuts of meat. Marinating, braising, or stewing can make tougher cuts more tender.
- Use canned fish such as tuna or salmon in sandwiches, chowders or a salad.
- Check store flyers for sales on cuts of meat that are typically more costly.
Load up on veggies and fruit
- Veg out! Most vegetables are low in carbohydrates and do not affect your blood glucose.
- Buy fresh vegetables and fruit when they are in season or on sale. If they are out of season, choose frozen or canned versions instead.
- Buy fresh produce at different stages of ripeness to enjoy it all week.
- Compare the price between fresh, frozen, and canned. They are all good choices.
.
Store your food wisely
Storing your groceries properly reduces food waste and saves you money. For instance, store your apples in the fridge. They soften ten times faster at room temperature (halfyourplate.ca/produce/fruits/apple/). For tips on storing fruits and vegetables, check the fruits and veggies section at halfyourplate.ca.
Preparing food to use later
If you buy food in bulk, or have more on hand than you can eat, prepare it for the freezer to use in the future.
- Wash and freeze berries and fruit for use in baking and smoothies. Yogurt can be frozen to use for baking and smoothies as well!
- Wash and freeze vegetables to put in stew, soup and casseroles. Use them to provide quick and healthy additions to your meals. For more tips on freezing food safely visit sobeys.com/en/articles/freezing-101/.
- When cheese is on sale, buy extra, grate it and freeze.
There is no easy solution for lowering your grocery bill. Like anything else in life, it takes a little planning, creativity and work. The rewards of better health and saving money are worth the effort.
Reviewed by: Laurie Barker Jackman, RD, a registered dietitian in Halifax, Nova Scotia and Margaret Young, RD, a registered dietitian in Kensington, Prince Edward Island.
Key points:
- If you’re living with diabetes, you’re twice as likely to develop heart disease.
- Heart disease can include heart attack, stroke, heart failure, irregular rhythm or beat (also called arrhythmia), and problems with the valves inside the heart.
- A healthy lifestyle and diet are your first line of defense.
The health of your heart directly affects the health of your entire body. As your heart pumps blood through your blood vessels, oxygen is supplied to your other organs, including your brain, and to every cell in your body. Conditions that affect the heart can make it less efficient in delivering oxygen. This can potentially harm the ability of other organs to function, and can lead to other diseases like kidney disease.
If you have diabetes, caring for your heart is very important. Those with diabetes are twice as likely to develop heart disease, and may experience it up to 15 years earlier compared to those who do not have diabetes. Heart disease affects about one in 12 Canadians aged 20 years and older. It is currently the second leading cause of death in Canada. Heart disease includes:
- heart attack
- stroke
- heart failure
- irregular rhythm or beat (also called arrhythmia)
- problems with the heart’s valves, which are inside the heart.
Does diabetes affect your heart?
Diabetes can lead to high levels of glucose in the blood. Over time, high blood glucose can damage the blood vessels throughout the body, including those of the heart. This high blood glucose can also damage the nerves that control the heart and other organs, leading to other health issues. Managing your diabetes with healthy lifestyle choices and medications will lower your risk of heart disease. The helpful actions you can take apply to both diabetes and heart disease, and so will benefit you in many ways.
How do I lower my risk for heart disease?
Some risks for heart disease cannot be controlled.
- Age: the risk of heart disease increases with age.
- Family history: if there is heart disease in your family, then it is more likely that you may develop it.
- Gender: men are more likely to have heart attacks compared to women. However, the risk for women increases after menopause.
Fortunately, there are risk factors for heart disease that you can control. The steps you take to protect your heart will also help with managing diabetes.
- Get regular physical exercise. The World Health Organization defines regular exercise as:
- 150 to 300 minutes of moderate to vigorous intensity physical activity each week or
- 75 to 150 minutes of intense activity each week.
- Exercise should include activities to strengthen muscles.
- Always speak with your health care professional before starting a new exercise series to ensure that it is right for you, especially if you have not been recently active.
- Avoid smoking. If you need help to quit, ask your health care team for assistance.
- Eat a balanced, healthy diet.
- Control your blood pressure.
- Control your cholesterol.
- Manage your blood glucose levels.
- Maintain a healthy weight, according to your body mass index (BMI).
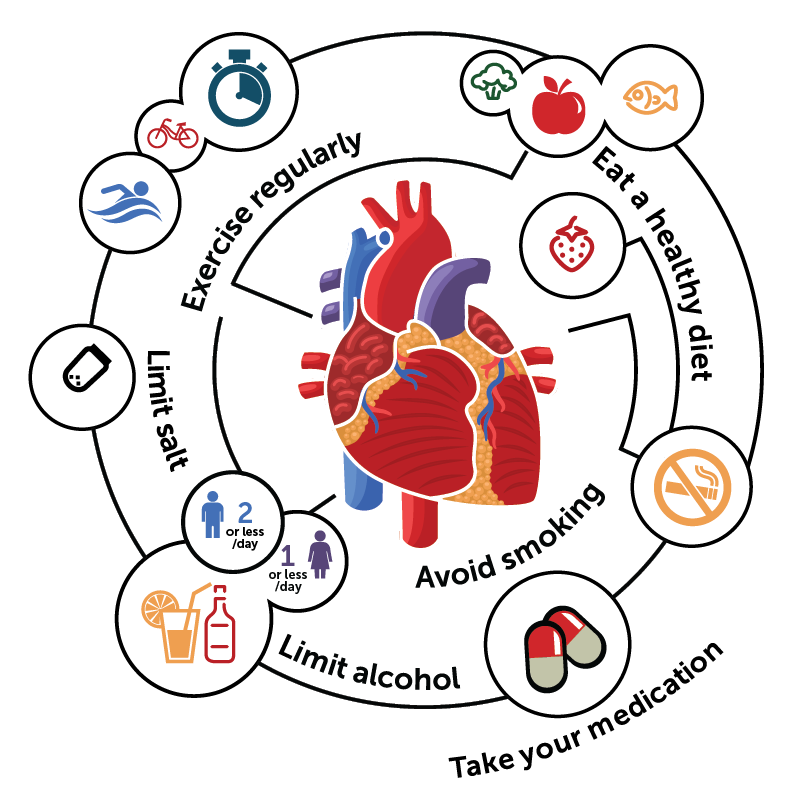
Tips for reducing blood pressure
You can lower your blood pressure and help reduce the risk of heart disease in many ways.
- Reduce salt intake. Excess salt can increase blood pressure.
- Exercise regularly.
- Do not smoke.
- Limit alcohol intake. Drinking in moderation means up to two drinks a day for men and one drink or less for women. If you do not drink, don’t start.
- Take the medication prescribed by your doctor to reduce your blood pressure. Check with your pharmacist to be sure you are taking your medication correctly.
- Eat a healthy diet. The DASH eating plan (Dietary Approaches to Stop Hypertension) has been shown to help lower or control blood pressure. It encourages choosing:
- foods low in salt and saturated fat (avoid fatty meats and full-fat dairy products)
- fruits and vegetables
- whole grain foods
- lean meats, fish, poultry, beans and nuts
- fat-free or low-fat dairy products
- foods rich in potassium, calcium, magnesium, fibre and protein.
About high blood pressure
One of the most important ways to lower your risk of heart disease is to control your blood pressure. Blood pressure is the force of blood pushing against your arteries as the heart pumps and as it rests between pumps. When blood pressure is too high for a long period of time, it can damage the blood vessels. Damaged blood vessels are less able to deliver blood to vital organs, including the heart.
High or uncontrolled blood pressure (hypertension) is one of the strongest risk factors associated with heart disease. Many scientific studies show that high blood pressure increases the risk for heart failure, irregular heartbeats, kidney disease, heart valve diseases, heart attacks, and strokes.
Many people cannot feel that they have high blood pressure, but sometimes they may be aware of chest pressure, chest pain, headaches, and vision changes. The only way to know for certain is by checking your blood pressure at your doctor’s office, at a local pharmacy or with a home monitoring device. If you are feeling fine but notice that your blood pressure is high or higher than normal, do not panic but follow up promptly with your doctor.
Different people, different blood pressure targets
There are two numbers in a blood pressure reading. The top (or first) number is the systolic blood pressure. This is the pressure of the blood pushing against the artery walls when the heart beats. The bottom (or second) number is the diastolic blood pressure. This is the pressure of the blood against the artery walls when the heart is at rest between beats.
A person’s ideal (or target) blood pressure will depend on their age and any risk factors they have, such as a history of diabetes, stroke, or heart disease. For example, the target blood pressure for an adult who has diabetes and high blood pressure is less than 130/80 mmHg.
If you have high blood pressure, your family doctor can determine what your blood pressure target should be, and can help you to reach your target.

Watch for these sudden symptoms of stroke:
- Numbness, tingling or weakness to one side of your body
- Confusion, difficulty speaking, or difficulty understanding speech<l/i>
- Severe headache
- Vision changes
- Trouble with walking, or problems with balance
Tips for Diabetes Injections

- Diabetes injections are easier and less painful than ever, thanks to thinner needles and insulin pens.
- Know which areas on your body are best for injecting each type of medication - and why it’s so important to choose a different spot each time.
- Insulin and other diabetes medications are delicate! Careful handling helps to make sure they work as expected.
If you live with diabetes, injected medication may be part of your treatment plan. Since insulin was discovered in Canada in 1921, it has both saved and improved the lives of people with type 1 and type 2 diabetes. When other injectable medications became available in Canada in 2010, people with type 2 diabetes gained more options to control their condition. Thanks to thinner and shorter needles, diabetes injections have never been easier or less painful.
A pen injection device can make injections much simpler than using vials and syringes. Pens have the added advantage of being less noticeable while in public. If you currently use syringes for insulin injection, talk with a member of your diabetes team about the possibility of using an insulin pen.
Brushing up on your injection technique may help to make the process more comfortable and effective. Your diabetes health care team, including your pharmacist, are your best source of information about how to inject these medications.
Steps for insulin injection
- Wash your hands with warm water and soap.
- Wipe the rubber seal on the top of the vial or pen with an alcohol swab.
- If you use cloudy insulin, such as NPH or premixes, gently mix it to suspend the insulin before an injection. Roll the vial or pen between your hands 10 times horizontally, then tip from end to end at least 10 times, to get an even mixture. However, do not shake the vial or pen too hard. This can damage the insulin.
- If you use an insulin pen, put on a new pen needle every time. Next, set the dial to two units of insulin and shoot it into the air. This removes any air from the pen and checks that your pen and needle are working. Now, set the dial to the dose that you need.
- If you are using a syringe, first inject the same amount of air as your insulin dose into the vial while it is right-side up. With the syringe still in the vial, turn the bottle upside down, and draw up about five units of insulin. Push this insulin back into the bottle to get rid of any small air bubbles. Do this once or twice, until you can see that there are no bubbles. Draw your insulin dose into the syringe.
- When using a 4 mm pen needle (the size recommended for most people), insert the needle straight in at a 90 degree angle, without pinching up a fold of skin. If you use a longer pen needle (5, 6 or 8 mm) or a syringe, you may need to pinch up a fold of skin to avoid injecting into your muscle. Your diabetes team can advise you on the best needle option and injection technique.
- Inject all of the insulin, then keep the needle in the skin for 10 seconds before removing it.
Pen needles and syringes should be used once only. Immediately after the injection, remove the pen needle from the insulin pen and put it in a sharps container. Used syringes also belong in a sharps container. Once the container is full, close it securely. Take it to your nearest Safeway, Sobeys, Thrifty Foods, Foodland, Freshco or Lawtons pharmacy for appropriate disposal and replacement with a new container. Ask your pharmacist for details.
Injecting other diabetes medications
GLP-1 receptor agonists are daily or weekly injections used to treat type 2 diabetes. These brand names are Ozempic, Trulicity, Bydureon, Victoza, Byetta, and Mounjaro.
Combinations of GLP-1 receptor agonists and long-acting insulin are daily injections, also used for type 2 diabetes. These brand names are Soliqua and Xultophy.
Most medications are supplied in a different pen device except Mounjaro which is currently available in Canada in single-use vials.
The procedure to inject these medications is similar to injecting insulin. However, there are a few differences.
- Mounjaro needs to be drawn up from a single-use vial with a syringe. First inject 0.5 mL of air into the vial while it is right-side up. With the syringe still in the vial, turn the bottle upside down, and draw up a small amount of Mounjaro (if using an insulin syringe, about 5 units). Push this Mounjaro liquid back into the bottle to get rid of any small air bubbles. Do this once or twice, until you can see that there are no bubbles. Draw up 0.5 mL (or 50 units if using an insulin syringe) into the syringe. There will be a small amount of liquid left in the vial as they contain 0.7 mL to make it easier to draw up the required 0.5 mL. This small amount is meant to be discarded. Please consult your diabetes team/pharmacist for training and syringe/needle recommendations.
- Only Bydureon has a mixing procedure. Please consult the product instructions.
- Each product in a pen requires a different procedure to prepare the pen. Some require a small amount of liquid to be shot into the air each time. Others only require this step when first starting a new pen. Some do not require this step at all. You can find the details about preparing your pen in the product instructions. Ask your pharmacist for help if needed.
- Some products use the same pen needles as insulin. Others include the needles in the package. Please discuss this with your pharmacist.
Carefully choose the place for the injection
Diabetes medication is best injected into one of three areas of the body:
- the abdomen
- the top and outer thighs
- and the back of the upper arms.
These sites all have a layer of fat under the skin (called subcutaneous fat) that allows diabetes medication to be properly absorbed by the body. The back of the upper arm is a difficult area to self-inject, and so should only be used when another person is giving the injection. The buttocks contain subcutaneous fat, and so insulin can be injected here as well. However, injections of other diabetes medications in this area are not recommended.
Heat and massage can affect how quickly insulin is absorbed. Avoid injecting insulin after a sauna or hot bath, and do not massage the area after the injection, as this can cause insulin to be absorbed more quickly.
Scars, moles, or the navel (belly button) absorb insulin poorly. Do not inject within five centimeters (two inches) of these areas.
Rotate diabetes injection sites
If insulin is injected into the same spot over and over, fat can build up under the skin. This lump of fat, called lipohypertrophy, may interfere with the insulin being absorbed properly. You could experience unexplained high or low blood glucose as a result. To prevent lipohypertrophy, choose a different spot to inject each time.
Each injection should be about two centimeters (the width of one finger) away from the previous one. Your diabetes team can provide you with a diagram explaining the most effective way to use an entire area, such as your abdomen or thighs, for injections.
Ask your diabetes team to check your areas of injection regularly for lipohypertrophy. You should also learn how to detect it on your own. If such an area is found, avoid injecting there. With time, the fat buildup under the skin will be absorbed and the area can be used for injections again.
Although GLP-1 receptor agonists do not cause lipohypertrophy, it is still important to rotate injection sites when using these medications.
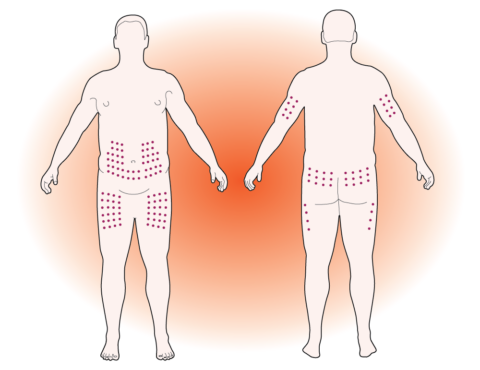
Recommended places for injection
Properly care for and store medications
Insulin and GLP-1 agonists are delicate. Special care must be taken to keep them safe. They should not be overheated, exposed to sunlight, frozen, or shaken roughly. Injectable diabetes medications that are not handled correctly can lose their effectiveness. Damaged medications may not be able to control blood glucose levels.
- Each multidose injectable diabetes medication is good for a certain number of days after opening. This will vary from 28 to 56 days, depending on the product. Please consult the product information.
- Once you open a multi-dose injectable diabetes medication pen or vial, keep it at room temperature. Injections will be more painful if the medication is cold.
- Store extra injectable diabetes medications in the refrigerator. Kept this way and unopened, they can be used until the expiry date. Always check the expiry date before you use a medication, and discard any that have expired.
- If required, Trulicity can be stored at room temperature for 14 days, Bydureon for 28 days, and Mounjaro for 21 days.
- If you plan to travel, discuss storage requirements with your pharmacist well ahead of your departure date.
- Medications that have been frozen, heated, or exposed to direct sunlight should be discarded.
For More Information
Diabetes Canada webinar, How to inject insulin – a step-by-step guide:
http://tiny.cc/how-to-inject
With education and practice, injectable diabetes medications can be used safely by anyone with diabetes. Regular review of your technique is a good idea. Members of your diabetes team, such as your diabetes educator or pharmacist, can help you to refresh your skills at your next visit.
WRITTEN BY: Rami Chowaniec, BScPharm, CDE, a pharmacist at Southgate Safeway in Edmonton, Alberta.
Treatment for severe hypoglycemia
- If you have diabetes, low blood glucose can quickly become an emergency. It’s important to act quickly.
- This step-by-step approach explains exactly what you need to do, and how others can help.
- Knowing what triggers low blood glucose can help you to avoid it.
Danielle has been working in the garden for a few hours when she starts to sweat and feel nauseous. Her hands are trembling, and she suddenly feels very tired. Danielle goes inside and sits down at the kitchen table. Her partner Joe notices that she looks pale and asks if she is feeling okay. When Danielle tries to answer, her speech is slurred. Joe quickly gets Danielle’s blood glucose meter and helps her to check her blood glucose. When he sees that the reading is 2.7 mmol/L, he gets four glucose tablets (Dex4) for Danielle to take.
Danielle has just experienced common symptoms of low blood glucose, which is also called low blood sugar or hypoglycemia. Managing diabetes involves maintaining stable blood glucose. Keeping blood glucose levels close to normal helps prevent long-term complications, but can also increase the risk of having low blood glucose. Recognizing and treating symptoms of low blood glucose quickly is critical to preventing severe effects.
What is low blood glucose?
Low blood glucose occurs when the glucose level in the blood falls below 4.0 mmol/L. When this happens, the body is not supplied with the energy it needs.
Why does low blood glucose develop?
Changes in everyday activities are the most common cause of low blood glucose.
These changes may include:
- taking too much diabetes medication
- missing or delaying meals or snacks
- eating too little food
- increasing physical activity
- drinking alcohol without eating.
Is low blood glucose linked to taking certain medications?
If you use one or more of the following medications to treat diabetes, it is possible for your blood glucose to drop too low.
- insulin
- insulin combination medications (Xultophy or Soliqua)
- glyburide (Diabeta)
- gliclazide (Diamicron)
- glimepiride (Amaryl)
- repaglinide (GlucoNorm)
Keep in mind that taking a higher dose of these medications can also trigger low blood glucose.
It is unlikely that you will experience low blood glucose symptoms if you:
- manage your diabetes through diet and physical activity alone
- or only use other diabetes medications (in pill or injection form) that are not on this list.
Steps for treating low blood glucose
Step 1
If you have symptoms, check your blood glucose. A level of less than 4 mmol/L is too low. If it is not possible to check, treat your symptoms as if you have low blood glucose.
Step 2
Eat or drink 15 grams of fast-acting carbohydrate, such as one of the following:
- 4 Dex4 glucose tablets
- ¾ cup (175 mL) juice or regular soft drink
- 3 teaspoons (15 mL) of sugar dissolved in water
- 6 Life Savers
- 3 teaspoons (15 mL) of honey
If you take acarbose (Glucobay), your options to raise your low blood glucose level are more limited. As this medication slows down the absorption of other fast-acting carbohydrates, you must use glucose tablets or 1 cup plus 1/4 of a cup (313 mL) of skim milk.
Glucose (dextrose) tablets work faster than other type of treatment to raise the blood glucose level. Keep these tablets readily available at home, at work, and with you at all times.
Are you caring for a child who has diabetes? Your diabetes educator can recommend the amount of fast-acting carbohydrate to treat low blood glucose.
Step 3
Recheck your blood glucose after 15 minutes. If it is still below 4.0 mmol/L, treat again with another 15 grams of fast-acting carbohydrate.
Until your blood glucose rises above 4.0 mmol/L, do not eat or drink anything other than the fast-acting carbohydrate. Low blood glucose can cause anxiety that may make you feel like you need to eat more right away. However, if you eat too much, your blood glucose may become very high.
Step 4
Once your blood glucose level is above 4.0 mmol/L, have your normal meal or snack if it is planned within the hour. If your next meal is more than an hour away, eat a snack with 15 grams of carbohydrate and a protein source. For instance, have six crackers with peanut butter or cheese, or half of a meat, peanut butter or cheese sandwich. This should prevent low blood glucose before your next meal or snack.
Steps for Injecting Glucagon
Note: Training on how to give a glucagon injection is required.
- Follow the instructions included with the glucagon kit to mix the powder and the liquid.
- Draw the mixed fluid up into the syringe.
- Inject the glucagon into the outer mid-thigh, through clothing if necessary.
- Dispose of the syringe in an approved sharps container.
Steps for Using Glucagon Nasal Powder (Baqsimi)
- Remove the shrink wrap on package by pulling on the red stripe.
- Open the lid and remove the device from the tube.
- Hold the device between your fingers and thumb, being careful not to push the plunger.
- Insert the tip of the device gently into a nostril.
- Push the plunger firmly all the way in.
- When the green line on the device no longer shows, the full dose has been given.
Remove the tip from the nose and dispose of the used device and tube.

How can I prevent low blood glucose?
- Learn how medication, food, and physical activity affect your blood glucose levels. Regular blood glucose checks can help you keep it under control. Staying aware of your blood glucose level allows you to adjust the amount of food and physical activity you get.
- Eat regular meals and snacks. Eat enough at each meal, and try not to skip or delay eating.
- To prevent low blood glucose on sick days, you must keep eating and drinking foods that contain carbohydrate. Talk to your diabetes educator about what to eat on days when you are not well.
- If you are more physically active than usual, be aware that low blood glucose can happen. Check your blood glucose level more often, and eat more food as needed.
- Always carry a fast-acting carbohydrate with you. Glucose tablets are not expensive and are easy to bring along. Pick up a few packages from your pharmacy and replace your supply as you use them.
Symptoms of low blood glucose
Although not everyone experiences the same thing, these are some of the signs of low blood glucose:
- fatigue
- dizziness
- confusion
- anxiety
- hunger
- weakness
- sweating
- trembling
- rapid heartbeat
- tingling or numb lips
A medical alert bracelet or other medical ID jewellery can speak for you when you are ill or unconscious, alerting others that you have diabetes.
What is the emergency treatment for low blood glucose?
Talk to those who might need to help you in an emergency. Low blood glucose can cause confusion, and you may not be able to treat yourself. Describe the symptoms to family, friends, and coworkers. Tell them how they can help. Educate them on how to use glucagon. Show them where you keep your emergency supplies. Explain that having low blood glucose may make you act as if you were drunk. Quick identification and treatment can prevent mild low blood glucose from becoming more serious. Very low blood glucose levels can cause unconsciousness or seizures.
Knowing the signs of low blood glucose helps to keep you safe as you try to achieve good blood glucose control. It is important to notice and quickly treat low blood glucose to stop it from becoming more serious. If you have concerns about low blood glucose, and especially if you are experiencing frequent episodes, consult your doctor, diabetes educator, or pharmacist.
Emergency treatment for severely low blood glucose
If someone is unable to swallow or becomes unconscious because of severely low blood glucose, immediate emergency aid is needed.
Treat the person immediately with glucagon. This hormone is used to treat severely low blood glucose. In Canada, it is available as a powder that can be used in two ways. It can be inserted into the nose (and does not need to be inhaled to work) or injected into the thigh, upper arm or buttock. Either form quickly raises the blood glucose level of someone who is unconscious.
As glucagon can cause nausea and vomiting, turn the unconscious person on their left side after the glucagon is given.
Call 911 or emergency assistance.
Once the person becomes alert and can swallow, a fast-acting carbohydrate should be given.
WRITTEN BY: Rami Chowaniec, BSc. Pharm, CDE, a pharmacist at Southgate Safeway in Edmonton, Alberta.
Gestational Diabetes

- Did you know that one form of diabetes only appears during pregnancy? The medical name for it is gestational diabetes mellitus (GDM).
- Between three to 20 percent of pregnancies are affected by gestational diabetes. (could use a visual for this - 3 to 20 out of 100)
- Once the baby is born, the diabetes usually goes away. However, you may develop another form of diabetes later in life.
If you are pregnant, you may be surprised to learn that you are at risk of developing a form of diabetes that appears only during pregnancy. Gestational diabetes mellitus (GDM) affects between three to 20 per cent of pregnancies, depending on risk factors. If you do have it, caring for your health is essential both for you and for your unborn baby.
Almost everything we eat is digested into glucose (sugar), which goes into the blood. Insulin, made by the pancreas, helps glucose move from the bloodstream into the body’s cells to be used as fuel.
During pregnancy, the placenta releases hormones that block the action of insulin in the body. Many pregnant people produce enough extra insulin on their own, so this is not a problem. However, if there is not enough insulin to deliver the fuel, high amounts of glucose remain in the blood.
If you have gestational diabetes, it is not your fault. However, since leaving too much glucose in the blood causes problems, you will need to care for yourself differently.
How is gestational diabetes diagnosed?
Since GDM may have no symptoms, it is recommended that anyone who is pregnant should be tested between 24 and 28 weeks of pregnancy. Your doctor will order this screening test, which is done in a lab. You will first be given a very sweet glucose drink. One hour later, a blood sample will be drawn from your arm. A positive test shows that you have a high level of glucose in your blood.
If the level is slightly high, another blood test may be needed. More blood will be drawn before and after you have an even sweeter drink to see how your body deals with a greater glucose challenge. After the second test, a definite diagnosis can be made.
What happens if I have gestational diabetes?
If your diagnosis is positive, you will be referred to a doctor who specializes in GDM. This doctor and a team of health care providers work with you to manage the diabetes. You will learn how to check your capillary blood glucose (CBG) levels to monitor your blood glucose at home. This check must be done four times per day, generally before breakfast and after meals. You will be told how long after meals to check your blood glucose.
More studies are needed on the benefit of continuous glucose monitoring (CGM) in those with gestational diabetes. Recommended CGM targets are not yet known.
Keeping a record of your blood glucose numbers will help you and your diabetes team. The home blood glucose numbers that contribute to a healthy pregnancy are:
| (before breakfast) | under 5.3 mmol/L |
| One hour after meals | under 7.8 mmol/L |
| Two hours after meals | under 6.7 mmol/L |
If you use insulin, aim to keep the number over 3.7 mmol/L.
How do I manage my blood glucose numbers?
Blood glucose is affected by how and what you eat. When you eat too much at once, it is hard for the pancreas to make enough insulin. To help your own insulin work more efficiently, it is better to eat small amounts more often. As part of your diabetes team, a registered dietitian works with you to create a meal plan. You will be given a three-meal and three-snack plan to help control your insulin levels. Sometimes, a short walk after meals is suggested to help keep blood glucose levels lower.
What if my blood glucose is still over the limit?
If diet and lifestyle changes cannot control your blood glucose, you may need insulin injections. Although most diabetes medications cross the placenta to the baby, insulin does not. You will be given an insulin pen (needle) and taught how to use it. This may sound scary, but is actually very easy to do. Insulin doses are calculated based on your daily blood glucose readings. Don’t worry – you will have help in learning about this process. You will be asked to test your urine for ketones. When the body is not getting enough food in the form of glucose, the breakdown of fat creates ketones. You will use ketone test strips, available from your pharmacy, to test your urine each morning. If ketones do appear, your meal plan or your amount of insulin will be adjusted.
What if I ignore this whole scary-sounding thing?
High levels of glucose in your blood can make your baby grow larger, and make giving birth more difficult. Preeclampsia (high blood pressure that occurs during pregnancy) may occur. The baby may not develop normally and could have problems, much like a premature baby might. With totally uncontrolled diabetes, there is a higher risk of a stillbirth. You and your baby may have a higher risk of health problems later in life, such as type 2 diabetes and heart disease.
If this feels overwhelming, remember that you are not alone. Your diabetes team will give ongoing support and teaching throughout your pregnancy. Happily, good blood glucose control usually results in a healthy pregnancy and baby.
Who is at risk?
You may have a higher chance of developing gestational diabetes if you:
- have prediabetes
- had gestational diabetes with a previous pregnancy
- are over age 35
- are obese (with a BMI of 30 or more)
- have a history of polycystic ovary syndrome
- are a member of a higher-risk ethnic group (African, Arab, Asian, Hispanic, Indigenous, or South Asian)
- have given birth to a baby that weighed more than 4 kg (8.8 pounds)
- have a parent, brother or sister with type 2 diabetes
- have darkening of the skin (acanthosis nigricans) in certain areas of your body
- use corticosteroid medication for chronic illness.
Does gestational diabetes mean my baby and I will have diabetes forever?
Your baby will not be born with diabetes. However, since this condition is hereditary, it is possible that your baby might develop diabetes later in life. Nursing shortly after birth and for at least four months is encouraged to help avoid low blood glucose in your newborn. It also reduces your baby’s risk of obesity and diabetes.
For the parent, diabetes typically goes away. Six weeks after delivery, you will have another blood test to make sure your blood glucose has returned to normal. However, your risk of developing diabetes down the road is much higher – as much as 60 per cent. It is important that you have a blood glucose check done yearly.
I had gestational diabetes. What can I do to prevent developing diabetes in the future?
A healthy lifestyle and staying in a healthy weight range can improve your chances of avoiding diabetes. Health Canada suggests spending at least 150 minutes per week doing an activity. Walking is a simple and inexpensive way to stay active after pregnancy. You can even take your baby with you!
- Wear runners or good walking shoes and start with 30 minutes, three days a week. Build up to 30 minutes, five days a week.
- Don’t stop for the winter – try a gym, get your own treadmill or stationary bike or join the mall walkers.
- Add resistance to your activity. For instance, use two-pound Velcro weights, one strapped to each wrist. These are available anywhere sports equipment is sold.
- Always talk to your doctor before trying any strenuous activity.
- Nutrition is also important. When you skip meals, the body’s metabolism slows down to deal with the reduced amount of fuel.
- Try eating smaller amounts more often to keep your metabolism working efficiently and steadily.
- Limit eating out and high-fat meals.
- Rather than frying food, try baking, barbequing, broiling or using a crockpot. Include fruits and vegetables with every meal and most snacks.
Diabetes Canada has a variety of resources in the Nutrition and Fitness section of their website. You can also use the search “gestational diabetes” to find details on diabetes in pregnancy.
While learning that you have gestational diabetes may come as a shock, know that you can handle it. Your healthcare team is available to help you along the way. The end result – your healthy baby – is worth the challenge of dealing with gestational diabetes.
WRITTEN BY: Candice Gale Slobodian, RN, CDE.
UPDATED BY: Aniket Paria, RPh, APA, CDE, a pharmacist in Medicine Hat, AB.
Managing Diabetes Highlights:
- Think of vegetables as the stars of your plate, and choose them most often.
- Divide your plate into quarters. Fill half with vegetables and fruit, a quarter with whole grains, and a quarter with protein.
- Aim for a healthy proportion of food types, rather than focusing on certain amounts.
- Meat, milk products, beans and lentils all count as proteins.
Including a variety of healthy foods in each meal helps us to eat and live well. These healthy eating tips are based on the most recent version of Canada’s Food Guide, a practical tool that promotes balance at every meal. It describes not only what to eat, but how we should eat. Eating a diet with more plants can lower the risk of chronic health conditions like heart disease, diabetes and certain types of cancer.
Canada’s Food Guide: food-guide.canada.ca/en
What’s new in Canada’s Food Guide?
If you grew up with older versions of Canada’s Food Guide, you’ll find a few changes. The most recent guide takes a broader approach, focusing on the proportion of foods rather than portion sizes. Divide your plate into quarters, and fill half your plate with vegetables and fruit, one quarter with whole grains, and one quarter with protein foods.
Another big change is that the familiar four food groups are a thing of the past. As well, you will no longer find recommended serving sizes or numbers of servings.
The guide also considers cultural preferences, food traditions and environmental impacts. It encourages families to enjoy food, eat together, cook more often, and be mindful of eating habits.
Boost your vegetables and fruit
Make vegetables and fruit the star of your plate. They should fill half of your plate at every meal. Vegetables and fruit are full of fibre, antioxidants, vitamins and minerals. Fresh, frozen and canned vegetables and fruits are all good choices.
- Make it easy. Buy ready-to-eat vegetables like cherry tomatoes, pre-washed salad greens and baby carrots. Look for pre-cut fruit and vegetables.
- Use frozen vegetable mixes in spaghetti, stew or slow-cooker recipes.
- Keep canned or frozen fruit on hand for fruit salad or smoothies.
- Add extra vegetables to casseroles and soup.
- Add dried fruit to cereal or oatmeal.
- Roast or grill vegetables and fruit for a new flavour. Try peppers, cauliflower, squash, peaches or pineapple.
Get the Guide: food-guide.canada.ca/en

Protein power
Two food groups – the former Milk & Alternatives and Meat & Alternatives – are now replaced by a quarter plate of protein foods.
The new guide suggests eating plant-based protein more often, but still includes fish, seafood, meat, poultry and eggs. Plant-based proteins include beans, lentils, nuts, seeds and soy products. They have less saturated fat and more fibre, and are easy on the wallet.
You can include more plant-based protein foods in your meals in several easy ways.
- Start small. Gradually increase plant-based protein sources at meals. Try swapping half the meat for plant-based protein like lentils or TVP (textured vegetable protein) in recipes.
- Plan one meatless meal during the week.
- Stock your kitchen with a variety of canned beans and lentils. Simply drain and rinse before adding to your recipes.
- Top salad and stir-fry with chickpeas, almonds or cashews.
- Stir black beans into your favourite rice dish or add to salsa for a more filling dip.
- Add dried lentils to homemade soup. They cook quickly without the need to presoak.
- Choose a flavored hummus as a dip for veggies.
- Snack on roasted chickpeas or soy nuts.
To make your heart happy and healthy, have a meal with fish or seafood at least twice a week, and choose lean cuts of meat or skinless poultry.
Although dairy products no longer have their own food group, they still have a place in Canadian diets as part of the quarter plate of protein foods. Dairy products, such as lower fat milk, yogurt, kefir and cheese, provide protein and important nutrients like calcium and vitamin D.
Go whole grain
- Fill a quarter of your plate with whole grains at meals.
- Choose breads made with 100 per cent whole grain.
- Try whole grain pasta instead of white.
- Use quinoa in place of white rice or noodles in cold salads.
- Enjoy popcorn as a snack – but watch the toppings and salt.
- Add barley, brown rice or corn to soups or salad bowls.
- Swap quinoa, barley, or oat groats for white rice in pilaf or risotto recipes.

Personalize it!
Canada’s Food Guide provides general nutrition guidance for healthy Canadians. If you have dietary concerns or a health condition, a registered dietitian can provide advice on how to personalize the guide to meet your needs. Registered dietitians are the only regulated nutrition professionals in Canada, with the unique education, training and experience to find food solutions that work for you and your family.
WRITTEN BY: Laurie Barker Jackman, RD, a registered dietitian in Halifax, Nova Scotia.

